Genetic Resources
Contents
- 1 Statement of Purpose
- 2 Introduction
- 3 Developing Policies
- 4 Funding and Budgets
- 5 Facility Management
- 6 Genetic and Genomic Collections Storage
- 7 Operational Best Practice
- 8 Genetic Sample Processing
- 9 Inventory Control and Data Management
- 10 Use of Collections
- 11 Health & Safety
- 12 Ethical and Legal Best Practice
- 13 Contributors
- 14 Source Material
- 15 Links
- 16 References
Statement of Purpose
This page presents standardized guidelines for the management of genetic collections associated with natural history collections. These recommended practices are informed by general standards for biorepositories and augmented by information unique to natural history collections with the goal of providing a foundation for those curating genetic samples. Information pertains to all aspects of genetic sample curation and will assist those in making decisions regarding how to collect, store, track, process, and distribute genetic specimen samples. These guidelines provide an organized method to evaluate the relative costs and benefits of various strategies and to prioritize potential improvements and minimize risks to genetic collections, which is applicable to both enhancing a single existing collection, as well as those forming a centralized repository composed of samples from multiple independent collections.
Introduction
Researchers associated with natural history museums have made the collection of genetic resources a priority due to their importance in molecular studies, but often the long-term curation of these collections is difficult due to decentralized curation over multiple storage locations and lack of community best practice guidelines for their stewardship. Unlike traditional natural history specimens, the research utility of genetic samples increases with lower storage temperatures and fewer freeze–thaw events and, in addition, their use is consumptive. Collection managers must, therefore, maximize the research potential of each sample by carefully considering use on a case-by-case basis. In addition, collection personnel must always balance institutional goals with the curation needs of their respective collections. Therefore, these recommendations can be broadly or narrowly applied, depending on the mission of the institution and other factors that influence the curation of genetic samples, including budget, staffing, and space.
Developing Policies
Many natural history collections have institutional guidelines that outline how traditional specimens should be curated, but these guidelines generally are not specific enough to address the special curation needs of genetic samples. To ensure that genetic samples are curated consistently for long-term preservation and use, all genetic repositories should develop the following:
- Standard Operating Procedures (SOPs)
- Comprehensive guide to operations
Policies and procedures should be written by those with experience in the management of the genetic collection and should comply with all governmental and regulatory requirements. All personnel should be trained using these written guidelines to ensure accuracy and consistency of procedures when working in the repository.
Standard Operating Procedures (SOPs)
The SOP document should outline or summarize:
- Tasks performed by the personnel of the repository
- Scope of activities performed
- How the collection satisfies the mission and goals of the institution
- Access to the collection
- Equipment and tools present
- Acquisitions
- Accessions
- Cataloging procedures
- Curation activities resulting from the near-exhaustive or exhaustive use of genetic samples (e.g., subsampling, deaccessioning)
- Storage and organization of relevant permits and acquisition documents
- Specific requirements for acceptance of genetic samples, including:
- - Provisions regarding acceptable sample types
- - Preservation methods
- - Storage containers
- - Sample organization (e.g., sample vials arranged numerically, data and vials submitted concurrently)
- Minimal requirements for associated data associated (e.g., submission method, acceptable formats, Darwin Core standards)[1]
- Loans/gifts (e.g., requirements for requesting genetic samples, procedures associated with the approval, explanation of fees)
- Information technology needs
- Mandatory training for personnel
- Health and safety programs
- Personal protective equipment (PPE) required
- Equipment monitoring
- Maintenance activities
- Backup precautions
- Emergency procedures
- Contact order for personnel in case of operational questions or emergencies
Guide to operations
A more comprehensive guide to operations should detail complete day-to-day collection procedures, including:
- Specimen processing (e.g., accessioning, cataloging, sample transfer, sample labeling, sample tracking)
- Temporary and long-term sample storage criteria
- Database procedures
- Detailed use of equipment (e.g., operation, calibration, certification, maintenance, repair)
- Subsampling procedures
- Shipment of loans/gifts
- Disposal of waste (including biohazards)
Funding and Budgets
The current and future potential of a collection for researchers conducting molecular studies is highly impacted by the efficient monitoring and storage of the genetic samples. To fulfill their research mission and ensure the long-term conservation of genetic collections, repositories must function efficiently, which requires dedicated and consistent funding. For those collections that are not centralized, the cost of curating genetic samples is often included in the overall budget for the institution or department, or funds come from personal research budgets [2]. Comprehensive and detailed budgets allow institutions to:
- Ensure that support from internal and external sources is sufficient to offset operational costs
- Understand the costs of maintaining their collections
- Make informed decisions regarding operations
Facility Management
Regardless of whether genetic collections are in separate locations in an institution or are housed together in a centralized repository, those curating these collections should clearly examine the storage conditions and address any issues related to the space(s). Addressing potential issues, such as restriction of access to collection rooms and/or cold-storage equipment, reorganization of equipment, improvements in lighting, upgrades to flooring, increased ventilation, and backup precautions, can ultimately improve the long-term preservation of genetic samples.
Access and security
Genetic samples have significant inherent value to research because they are often collected from remote locations as a result of costly and time-consuming collection trips. Samples should, therefore, be stored in secure locations to minimize misplacement or inadvertent loss, and their access and use should be limited to those with the appropriate training. A risk assessment should be conducted to assess both building and collection security, including current procedures and protection devices. Many genetic collections currently store samples in a room or facility that remains unlocked during the day, which is likely because many research collections are stored within college and university laboratories allowing student access [2]. If access to rooms where genetic resources are stored must remain unimpeded, individual freezer units can be locked with key access restricted to approved and trained users. Policies should be developed in relation to visitors to ensure that they have the appropriate training before working with collections (see OPERATIONAL BEST PRACTICE: Training). Records of training and activity in the collection areas should be maintained and archived for security, as well as health and safety requirements (see OPERATIONAL BEST PRACTICE: Records Management).
Space planning
Space planning encompasses the organization of equipment (e.g., storage units, tools), adequate workspaces, and storage for supplies, in addition to the collections themselves. Although the layout of a functioning work area might not be greatly altered for an established collection, minor changes can be made to the placement of laboratory tables, desks, shelving, biosafety cabinets, or benchtop equipment (e.g., centrifuges, electrophoresis equipment, incubators, rockers, scales, spectrophotometers, tabletop autoclaves), that can increase research efficiency or improve functioning of equipment. Understanding every procedure that will be undertaken in the space will allow more accurate organization of the space, which is essential for those designing a centralized repository, as well as those working to improve the organization of a single laboratory. The inclusion of dedicated space for working with genetic samples or hazardous chemicals (e.g., biosafety cabinet, chemical hood, designated laboratory bench, room) is recommended to protect both personnel and samples.[3]
Open spaces must be reviewed along with dedicated storage areas to:
- Ensure that mechanical refrigerator and freezer units are placed to allow for adequate airflow
- Avoid obstruction of exits, access or equipment (e.g., fire extinguishers, eyewashes, safety showers) by dedicating spaces for mobile equipment (e.g., laboratory carts, dewars/cylinders of LN2)
- Consider facility and/or safety issues associated with routes traversed for specimen transport, maintenance of equipment, and delivery of dewars of LN2, including:
- - Elevators (e.g., personnel may not transport pressurized dewars in elevators if ventilation does not accommodate oxygen deficiencies)
- - Steep inclines
- - Floor surfaces
- - Movement through populated and public areas
Lighting
Lighting in the collection space should be sufficient to allow personnel to complete small-scale tasks, including:
- Examining vials for cracks
- Reading hand-written or typed labels on containers
- Subsampling specimens
If the light source is in close proximity to frozen samples (i.e., task lighting), a lighting unit that generates minimal heat (e.g., florescent fixtures, LEDs) should be used instead of incandescent or halogen lighting because these latter can cause samples to thaw. Emergency lighting that functions in the event of power loss should also be present to illuminate exit routes and, if needed, allow personnel to monitor cold-storage equipment (see FACILITY MANAGEMENT: Backup Precautions). Focused, portable light sources (e.g., flashlights, headlamps, battery-powered lanterns) should also be readily available within the collection in case of emergencies or if needed to examine equipment.
Flooring
Flooring used in genetic repositories should be durable enough to accommodate all activities performed in the space and be:
- Washable
- Able to support heavy cold-storage equipment without cracking
- Level so as not to obstruct the movement of equipment, including laboratory carts and dewars (cylinders) of LN2
- Compatible with LN2 so cracks do not occur with spills or leakage. Additional notes regarding flooring and LN2:
- -Vinyl tile and linoleum are not recommended with the use of LN2 because they can crack and lift, presenting a hazard.
- -Sealed concrete is recommended over epoxy because if LN2 is spilled on the latter, it can break the seal between the epoxy and concrete, causing cracking
If harder surfaces, such as concrete, are selected because of their durability, anti-fatigue mats should be placed in areas where personnel stand for prolonged periods of time for potential ergonomic issues. Additionally, absorbing mats or floor grates might be needed in the front of refrigerator condensers or in the vicinity of freezers to protect personnel from slipping on occasional condensation or ice.
Ventilation
Ventilation must be adequate in all collection spaces to prevent excess heat or humidity, which cause mechanical units to overheat and create condensation that damages equipment and results in an electrical shock hazard. More importantly, ventilation must consistently maintain sufficient oxygen levels if using LN2. Using liquid nitrogen for maintaining genetic collections requires constant monitoring of oxygen levels because nitrogen is a colorless, odorless and tasteless gas/vapor that is an asphyxiant, causing oxygen depletion. If LN2 leaks into an enclosed space from a defective cryovat or supply dewar, oxygen levels might become depleted enough to be unsafe for occupants (see HEALTH AND SAFETY: Liquid Nitrogen Safety).
To understand potential oxygen depletion due to LN2 use in a genetic collection, the normal evaporative losses from storage vessels and the spillage of the entire contents of a vessel should be estimated for each collection room. Potential oxygen depletion can be determined by analyzing the following:
- Size of the room
- Evaporation loss for each vessel (reported by the manufacturer as ‘‘volume of LN2 lost per day’’)
- Total spillage of each vessel
- Number of air changes in the room per hour
If neither normal evaporation losses nor spillage cause a significant reduction of oxygen content in a room, then general exhaust ventilation or use of natural ventilation (e.g., opening doors, windows) can be considered as an option. Natural ventilation is not always possible, however, because of institutional restrictions or special designations (e.g., Biosafety Level 2 or 3) requiring that windows are sealed and/or doors shut. If risk assessment calculations of potential oxygen depletion indicate that evaporation losses and/or spillage would significantly deplete oxygen concentrations, forced-air ventilation must be installed. For accuracy in such high-risk matters, a professional engineer should be contacted and the health and safety group of the institution consulted.
Forced-air ventilation can include the following:
- Extractor fans that run continually, providing 100% exhaust and assuring that none of the cycled air is returned back to the air handler
- Fans that are activated manually by the user when alerted that oxygen levels are low
- Fans that are activated automatically by an automatic trigger
Fans that use an automatic trigger are recommended over those with manual activation to remove need for human intervention to correct oxygen levels. Automatic activation of an extractor fan can be linked to sensors that detect room occupancy and/or oxygen levels (see FACILITY MANAGEMENT: Oxygen Monitors). Having both occupancy sensors and oxygen levels activate an extractor fan serves as a safety redundancy should one sensor fail. Regardless of the type of ventilation system chosen, exhaust systems should include forced extraction ducts that are installed at low heights close to the floor because cold nitrogen vapors are denser than ambient air and settle at floor level. Exhaust ducts should also be in close proximity to storage units for the most efficient removal. With all ventilation systems, noise exposure from fans must fall within limits recommended by the Occupational Safety and Health Administration (OSHA), and collection managers should contact their environmental health and safety group to evaluate the noise levels and attenuate the fans if needed.
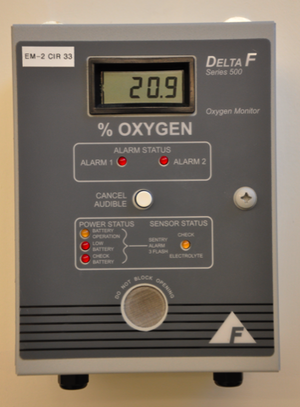
Oxygen monitors
Ambient air normally contains 20.9% oxygen by volume, but nitrogen gas can quickly displace the air in the event of a spill or failure of storage equipment, reducing the percent of oxygen to unsafe levels. By OSHA standards, a ‘‘hazardous atmosphere’’ can include one that is oxygen-deficient, containing less than 19.5% oxygen by volume. This type of environment exposes people to the risk o incapacitation, injury and possible death. Oxygen monitors should, therefore, be present in all rooms where LN2 is stored or dispensed, and these monitors are essential in rooms where personnel are working with LN2 storage equipment. Some ventilation systems using extractor fans can be automatically activated using oxygen levels; these systems can operate independently or be tied into the general room oxygen monitors (see FACILITY MANAGEMENT: Ventilation). Oxygen monitors can be either portable or permanently installed within the collection space:
- Portable monitors are small, light-weight, and can be carried by individuals working in a room with LN2 equipment
- Permanent installations (i.e., battery operated, electrical units) ensure constant and consistent surveillance of oxygen levels
- - Displays should be mounted approximately at eye level
- - Oxygen sensors should be positioned closer to floor level but above the level of any exhaust-extraction fan located in close proximity
- - Additional alarms in adjacent rooms or hallways are recommended to prevent personnel from entering an oxygen deficient areas
- - Alarm notification to a remote location is a worthwhile precaution so emergency personnel and those responsible can be alerted to problems.
Regardless of whether these devices are fixed or mobile, oxygen monitors should include both audible and visual alarms. To assure that oxygen monitors comply with local regulations and function accurately, a professional engineer should be contacted and the health and safety group of the institution consulted. In addition, some electrochemical sensors used within oxygen monitors are sensitive to the surrounding environment and are subject to drift with barometric changes or can even fail if placed in extremely cold temperatures. Therefore, dedicated maintenance, periodic calibration and regular replacement of sensors is essential for all collections using LN2.
Backup precautions
Collections that use cold-storage units to store genetic samples should include backup precautions to protect against power loss and ensure constant temperatures, thereby preventing sample loss.[4] Backup precautions are the necessary counterpart to a monitoring program, which protects samples from loss due to specific equipment failure (see OPERATIONAL BEST PRACTICE: Manual Monitoring). Fortunately, audible or visual alarms are included in many cold-storage units, but are merely the first step in protecting genetic samples. A risk assessment should be conducted to determine the appropriate backup system given the following:
- Cold-storage type (e.g., refrigerator, mechanical freezer, LN2 cryovats)
- Institutional infrastructure (e.g., available backup power sources)
- Regional factors (e.g., risk of severe weather, proximity to populated areas)
- Running duration of each type of backup system
Automatic systems are recommended over those that must be activated manually to ensure that collection storage equipment remains functional at all times, even when personnel are not readily available. It is also recommended that equipment alarms include both on-site and off-site notifications. Off-site alarms include 24-hour monitoring and ensure that the appropriate personnel can be contacted at any time in case of emergency. Contact information for multiple staff members trained to respond to emergencies should be included in the SOP document and posted within the collection to ensure that emergencies and alarms are addressed appropriately and immediately. Written emergency procedures should address how personnel should respond to various situations (see OPERATIONAL BEST PRACTICE: Emergency procedures).
As part of a risk assessment, collection managers should identify what equipment is essential and requires backup power in the event of power loss. Risk assessments should be conducted regularly because contents of individual cold-storage units can change, which might alter priorities for backup power. Mechanical freezers should always be connected to backup power. Managers of collections using LN2 storage units should consider having backup power for the LN2 cryovat controllers to ensure that cryovat units continue to receive LN2 supply from dewars when the commercial power is not present; however, the addition of LN2 can be done manually if needed (see GENETIC AND GENOMIC COLLECTIONS STORAGE: Liquid nitrogen cryovats). Environmental monitoring systems and safety equipment, such as oxygen sensors, specialized ventilation, and emergency lighting, should also be protected by backup measures.
If regular power is lost, an auxiliary or emergency-power system can automatically connect to emergency power. Most emergency-power systems use diesel, natural gas, or liquid propane gas-driven generators to power essential equipment in a facility. Managers evaluating emergency-power systems should consider the following:
- Multiple generators might be necessary to support large collections if many mechanical freezers are present.
- Enough fuel should be present to sustain power continuously for at least 48–72 hours, but there also should be an established plan for how fuel supplies can be replenished if needed. [5]
- An uninterruptible power supply (also called uninterruptible power source, UPS) or battery/ flywheel backup can also provide short-term emergency power if commercial utility power fails. In an emergency situation, these units can provide personnel with essential time to connect to other secondary power sources, such as backup generators. In addition, some mechanical freezers require users to manually restart the unit after a power failure to protect the compressors, and an UPS would make this restart unnecessary.
- Power systems should be stored in an easily accessible and dedicated storage space so collection personnel can access them when needed.
- All backup power systems should be tested on a regular basis as part of the SOP to ensure that they function and can sustain the electrical load in an emergency.
Genetic and Genomic Collections Storage
The type of storage used in a genetic or genomic collection ultimately influences the potential future uses of samples in molecular research because colder temperatures reduce cellular degradation. Documentation of the number of freeze–thaw events and any chemical preservatives or buffers should also be considered because genetic sample integrity might be reduced, depending on the preparation, as well as the duration and number of freeze–thaw cycles. Collection managers should also track all storage methods utilized from the time of initial collecting and any usage events (i.e., loans/gifts).
Temperature considerations
Cryopreservation at very cold temperatures is considered the most effective technique for the long-term stabilization of genetic samples because it inhibits enzymatic and chemical activity that leads to sample degradation [6] [7] [8] [9] [10]When genetic sample temperatures are reduced below -137°C (the vitrification point of water), biological activity substantially slows and, at -196°C (the boiling point of liquid nitrogen), DNA degradation virtually stops because there is insufficient thermal energy for chemical reactions. Thus, the type of cold storage chosen for samples affects the long-term viability of those samples, with the most reliable form of cryogenic preservation being the storage of samples at temperatures below -137°C and improving as storage temperatures decrease below this threshold. However, collections might include genetic samples preserved in a number of ways, given size of the collection (including estimated future growth), personnel, funding, dedicated space for equipment, and ength of time the samples will be stored.
In addition to long-term storage in a collection, there must be considerations for short-term storage situations in relation to when samples are collected and transferred, such as for loans/gifts. Various methods, including freeze-drying samples or preparing them using buffers, chemical preservatives, or desiccants, are currently used for the initial preservation of genetic samples. [11] [12] [13] These methods, which generally allow genetic samples to be stored at room temperature, are most appropriate for short-term storage or transport and not for long-term preservation (see GENETIC SAMPLE PROCESSING: Initial preservation procedures). Long-term viability can be increased for genetic samples initially preserved using these methods if they are ultimately stored in a low-temperature environment. In general, genetic samples should be stored at the lowest temperature possible at any available time to reduce degradation and maximize future use.
Liquid nitrogen cryovats
Liquid nitrogen cryovats are cryogenic freezers that are cooled in various ways using a supply of nitrogen in the liquid phase. All methods of cryopreservation that use LN2 are considered to be the most effective because samples are stored at temperatures below the glass-liquid transition temperature of water (-137°C). There are currently four different storage methods that use LN2:
- Vapor-phase cryovats with LN2 present below sample racks (≤-150°C; most commonly used method by collections surveyed[2])
- Liquid-phase cryovats that allow submersion of samples in nitrogen (-196°C)
- Isothermal cryovats with a specialized jacket surrounding the interior chamber and allowing nitrogen vapor to enter the freezer space via directional vents (approximately -190°C)
- MVE Vario cryovats (-50°C to -150°C) that allow LN2 to flow through a heat exchange system located in the top head of the freezer, using vaporization energy of the LN2 to cool the unit
All four types of cryovats are available in various sizes with vial capacities that range from approximately 20,000–100,000. Use of liquid-phase cryovats are not recommended because nitrogen in a liquid state can penetrate all commercial cryogenic vials if not placed in secondary containment (e.g., polyethylene tubing), making them at risk of exploding when they expand upon warming (see GENETIC SAMPLE PROCESSING: Storage containers). In addition, cross-contamination can occur when immersing samples directly in LN2 without securing the cryovial in secondary containment.[14] The circulation of vapor within isothermal cryovats allows for improved visibility due to less clouding at the top of the chamber, but these cold-storage units have increased consumption of LN2 when compared to traditional vapor-phase cryovats. MVE Vario cryovats are the newest freezer systems, having the benefit of a dry storage area, but this technology is not yet used or tested by natural history collections.[2]
Most liquid nitrogen cryovats are equipped with electronic controllers that automatically monitor and regulate the supply of LN2 to the unit. Liquid levels, temperature readings, and alarms are generally displayed on a controller unit panel. Cryovats with electronic controllers generally use a two-sensor system to detect LN2 at user-defined levels. When LN2 levels are below the low-level sensor, a solenoid valve is opened, allowing product to enter the cryovat from a nearby source (e.g., small-volume dewar, large volume bulk tank) connected via a cryogenic hose and/or vacuum-jacketed piping (see GENETIC AND GENOMIC COLLECTION STORAGE: Liquid nitrogen supply). When LN2 levels reach the high-level sensor, the solenoid valve is closed, stopping the flow of product into the cryovat. In addition to both on-site and remote alarms, it is paramount that cryovats are checked at regular intervals and levels of LN2 are recorded (see OPERATIONAL BEST PRACTICE: Manual monitoring). When using LN2 cryovats, backup power for the electronic controller functions to keep a continuous supply of LN2, although the unit itself stays cold without power (see FACILITY MANAGEMENT: Backup precautions). If a cryovat controller unit that automatically dispenses LN2 is not connected to a backup system, readings of LN2 levels and the addition of more product (i.e., pouring LN2 into the cryovat) need to be done manually; LN2 would likely need to be supplied at regular intervals to maintain ultracold temperatures if power remains off for an extended period of time. In the event of a power failure, collection procedures should detail if and when cryovat lids are opened to minimize use of LN2 (see OPERATIONAL BEST PRACTICE: Emergency procedures).
Liquid nitrogen supply
Liquid nitrogen to supply cryovats can be obtained and stored in three ways:
- Delivery in small-volume dewars (cylinders)
- Delivery to large-volume bulk tank
- Self-production using an on-site LN2 plant
Delivery in small-volume dewars (cylinders) by a commercial vendor can be done needed on a regularly scheduled basis. For most small collections, mobile dewars (up to 240 liters) are sufficient to supply cryovats. Dewars are generally placed in close proximity to the cryovats and connected with cryogenic transfer hoses, unless permanent vacuum-jacketed piping designed to transfer cryogenic liquids is installed within the repository. Dewars themselves can be purchased and refilled by a delivery vehicle, or these storage vessels can be leased so that an empty dewar is exchanged for a full one. In addition, Department of Transportation (DOT) codes regulate the specifications of liquid nitrogen delivery vessels in the USA, so collection managers should be aware if these regulations affect their delivery. LN2 deliveries should be scheduled to minimize the amount of time that a dewar is not connected to a cryovat to ensure that a cryovat has a steady supply of LN2.Collection managers should be aware that LN2 evaporates at a constant rate, which can be affected by the atmospheric conditions, vessel integrity, and manufacturing tolerances.
For large collections with many cryovats, a pressurized bulk or microbulk tank should be considered. Depending on the size of the bulk vessel, the tank might need to be located outside of the building where the collection is housed. If bulk tanks are placed indoors, itmight be possible for external wall boxes to be installed to allow bulk tanks to be filled without having to enter the building. Costly vacuum-jacketed cryogenic pipes are needed to deliver the LN2 from the tank to the point of use, so for cost efficiency, bulk tanks should be located as close to the cryovats as possible. In many areas, bulk tank storage is regulated by city or state ordinances; oxygen monitors are also essential if these storage units are placed indoors (see FACILITY MANAGEMENT: Oxygen monitors).
In smaller collections that are located in remote locations where LN2 cannot be easily delivered, collection managers might consider the use of LN2 plants, which generate nitrogen by separating it out from the ambient air. The plant-generated LN2 is stored in a tank that then can be moved and connected to a cryovat.
Mechanical freezers and refrigerators

Mechanical freezers and refrigerators offer a large range of storage temperatures, including ultracold freezers (-50°– -86°C), general-purpose or laboratory freezers (-12°– -30°C for manual defrost models; automatic defrost models allow temperatures to fluctuate more broadly), and general-purpose refrigerators (1°– 12°C). As previously discussed, cryogenic storage at extremely low temperatures is considered the most effective method for the long-term stabilization of genetic samples. However, refrigeration is sometimes considered for short- or long-term storage if certain buffers or chemicals were used in sample preservation, and these additives only require that genetic samples be kept below ambient temperature. Collection managers must record all chemical additions and preservatives used with their genetic samples to ensure that the samples are stored at the appropriate temperature recommended by the manufacturer. If multiple cold-storage methods are used within a collection, the SOP should clearly outline the criteria for storing samples at the different temperatures.
Freezers and refrigerators are available in a variety of sizes, styles, and voltages, including upright or chest configurations. Many models are available with locks for additional security (see FACILITY MANAGEMENT: Access and security). Collection managers should ensure that each electrical unit has a dedicated circuit so power is not overloaded, and that units are positioned to allow for sufficient airflow around them (see FACILITY MANAGEMENT: Space planning). Heat released from cold-storage equipment should be monitored and counter-balanced by an HVAC or cooling system when needed. Those collection managers purchasing new equipment should consider freezer units that have increased energy efficiency, which generally ensures that less heat is emitted to the surrounding air. Compressors can also be placed outside of the building for some freezer units, removing the need for HVAC or cooling in the collection space where the mechanical freezer is located. Fortunately, compressor systems on newer cold-storage units include those being cooled by water, whereby valves connected to local water sources automatically control the flow needed to maintain cooler compressor temperatures, which enhance the stability and reliability of the unit. Because cold- storage units are integral to the functioning of a genetic or genomic collection, the SOP should outline specific protocols for regular preventative maintenance and emergency repair of all mechanical units (see OPERATIONAL BEST PRACTICE: Equipment preventative maintenance, repair, and replacement).
Mechanical freezers and refrigerators require less dedicated time in their day-to-day operation when compared to LN2 cryovats, but collections have an increased risk of loss in the event of mechanical breakdown or power disruption. Even a short power outage can be detrimental to samples being stored in a mechanical cold-storage unit. Battery backup systems or an UPS are needed to maintain units in the event of a short power outage or until power can be switched over to a robust backup system for longer term emergencies (see FACILITY MANAGEMENT: Backup precautions). Internal and, if possible, remote monitoring should be present to prevent sample loss due to mechanical failure of units (see OPERATIONAL BEST PRACTICES: Manual monitoring). To safeguard against all possible risks, including power outage and mechanical failure, both monitoring procedures and backup precautions should be clearly outlined in the collection SOP.
Operational Best Practice
Genetic and genomic collections are more equipment- and personnel-dependent than traditional natural history specimens, with more catastrophic consequences if storage equipment fails or samples are handled improperly. In addition, genetic samples are consumable resources, so they become more limited with each use for research.
Facility functions and services provided
Genetic resource collections can provide many key services to fulfill institutional missions and assist internal and external researchers in achieving project goals. How broadly and consistently these key services can be addressed is related to how genetic collections are set up at an institution (i.e., separate locations or centralized facility). The main functions of most centralized genetic resource facilities associated with natural history museums include [2]:
- Sample storage
- Sample tracking
- Sub-sampling and/or processing of loans/gifts
A small percentage of repositories provide additional genetic laboratory functions, including DNA/RNA extraction, polymerase chain reaction (PCR), and sequencing.[2]
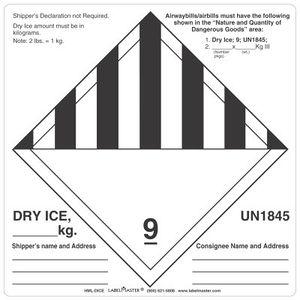
Besides genetic sample maintenance, additional research services could potentially be provided by genetic resource collections, including assistance with project planning or proposal submissions, sample collecting, assistance with sample transportation from the field, sample quality assessment using spectrophotometry or other methods, and student or intern training.[15] Collections could also provide or lend supply materials for those researchers who will be depositing samples in the biorepository, including sample vials, sample boxes, reagents, LN2 dewars, dry shippers, LN2, or dry ice. To ensure that sufficient equipment, supplies, trained personnel,and funding to maintain high-quality specimens are available, and to potentially offer additional services, collection managers should clearly outline priorities, as well as the molecular laboratory tasks performed by collection staff (e.g., DNA/RNA extractions, fluorometric/spectrophotometric quantification of DNA, DNA barcoding to identify or confirm identifications) in the SOP document.
Personnel
Genetic and genomic resource collections must be managed properly and continuously to ensure that samples are properly stored and maintained. Depending on the size of the collection and institution type, personnel might include a single manager or numerous employees. A recent survey of genetic resource collections associated with natural history museums found that the vast majority had curators/professors with higher academic degrees or collection managers with higher degrees maintaining the collections [2]. Other personnel working with genetic resources included:
- Collection managers without higher degrees
- Staff or technical assistants
- Paid and unpaid student assistants
- Volunteers
At minimum, collections staff should include a dedicated manager who is trained to manage the day-to-day activities within the collection and can ensure that all procedures are completed as instructed in SOP documents. A collection manager also prevents unauthorized access to storage areas, thus protecting samples from misplacement, accidental thawing, or contamination[16]. Duties and reporting relationships for each staff member should be clearly outlined in a written job description. Collection managers should ensure that all personnel working in the collection have the appropriate training to undertake the duties assigned in their particular job description, especially with regard to health and safety issues. Proper maintenance of genetic resource also requires assistance from additional departments outside of those working directly with the collection, including building maintenance and operations, environmental health and safety, information technology, and security.
Training
All genetic collection staff must receive adequate training to ensure that they can perform all aspects of their job description and follow all policies and regulations, including those mandated by international, national, regional, and local statutes. All new personnel, including staff, students, interns, and volunteers, should be trained by authorized staff to understand the details and justification for the SOP documents and comprehensive protocols. Policies should also be developed in relation to both short-term and long-term visiting researchers to ensure that they have the appropriate training before working with collections. Training should include the following:
- Best practice for working with genetic resources (see GENETIC SAMPLE PROCESSING: Sample transfer; USE OF COLLECTIONS: Aliquoting samples)
- Database usage and the proper storage of samples in accordance with corresponding database records (see INVENTORY CONTROL AND DATA MANAGEMENT: Databasing for genetic samples)
- Safety and security, including the appropriate use of tools and equipment, proper personal protective equipment, and risks of working with chemicals and biospecimens
Internal records should be kept of all approved personnel and dates of their various training events, especially because some training requires mandatory updates at regular intervals. All training programs should be regularly assessed to make sure that information is up to date, and it is recommended that training be done in collaboration with the health and safety group at the institution.
Manual monitoring
The viability of genetic samples is dependent on storage equipment operating at optimum efficiency. Collection procedures should clearly outline how to monitor and check collection equipment, how often it should be done, and how to maintain documentation. Diligent and consistent monitoring of the following equipment should be completed:
- Cold-storage equipment
- - Personnel should visually inspect and record the temperature of the equipment on a regular basis (e.g., daily, multiple times per week).
- - Levels in liquid nitrogen cryovats should be measured manually on a regular basis to confirm that the measured levels match the control displays
- - Temperature and nitrogen-level data should be tracked on a regular basis to identify problematic trends
- Transportable pressurized vessels, including dewars (cylinders) of LN2, should be examined upon receipt from outside vendors
- - Dewars should be checked to ensure that pressurization is compatible with the cold-storage equipment
- - Dewars should have no be visible damage or leakage
- - When in use, these vessels should be closely monitored to estimate rate of use and ensure that valves are functioning properly
Equipment preventative maintenance, repair, and replacement
Proper functioning of cold-storage equipment is essential for the long-term stability of genetic material. All equipment should have regular routine maintenance in accordance with the recommendations of the manufacturer. Preventative maintenance of mechanical freezers should include:
- Comparing the temperature set-point versus the actual temperature (see OPERATIONAL BEST PRACTICE: Manual monitoring)
- Testing backup batteries
- Ensuring that gaskets and seals are intact without tears
- Routine cleaning of freezer coils and condenser filters
- Regular defrosting
In addition to increased dependability, regular maintenance of cold-storage equipment, such as mechanical freezers, is associated with significant energy savings.
Liquid nitrogen cryovats should have routine maintenance to ensure:
- Internal temperature sensors function properly
- LN2 readings are accurate
- Fill valves operate normally
- Alarms activate under the defined conditions
- Insulating materials (e.g., polystyrene foam) do not have cracks or built-up frost
- No ice or frost build is present in sensor tubes
Biosafety cabinets and chemical fume hoods should be tested and certified routinely to ensure that they are functioning appropriately and in compliance with both local regulations and any requirements associated with biosafety level status. Oxygen monitors also need regular maintenance and/or calibration as life safety equipment (see FACILITY MANAGEMENT: Oxygen monitors). All safety equipment, including eyewashes, safety showers, fire detection units, and fire suppression systems, should be tested regularly to ensure reliability, which is generally best accomplished in collaboration with the health and safety group of the institution. Managers should keep records of all routine and special maintenance, including dates, description of the issues (e.g., alarms, incident reports), tests performed, and actions taken to resolve any problems. The SOP should provide plans, including instructions and schedules for preventative maintenance, calibration, repair, and replacement of equipment.
Regular assessments of equipment should be made by collection managers to help establish a timeline for replacement. Mechanical freezers generally last from 5 to 15+ years with manufacturers reporting a range of 8–12 years, whereas liquid nitrogen cryovats generally last longer, functioning for 10–35 years [17]. Collection managers should track the ages of all equipment and know the manufacturer’s expected lifespan for each. Based on the age and performance of the equipment, long-range plans for replacement can be anticipated and replacement funding can be ensured. If a cold-storage unit should fail, written procedures should be in place to identify how to transfer the samples from the failed unit to their emergency storage location (see OPERATIONAL BEST PRACTICES: Emergency procedures).
Records management
Collection managers should maintain records that detail collection, processing, storage and use of samples. Copies of all relevant permits and acquisition documents, which detail the legal attainment of all genetic samples either alone or associated with traditional voucher specimens, must be maintained for both legal obligation and assessment of the sample history and quality. Up-to-date records should be available that document personnel training, equipment activity (e.g., monitoring, preventative maintenance, repairs), safety inspections, and legal compliance (e.g., active permits) as outlined in the SOP.
Genetic sample data can be recorded as part of an institutional database, which potentially tracks both the original voucher specimen and any subsequent associated genetic or genomic derivatives, or a stand-alone tracking system that is used only for genetic samples (see INVENTORY CONTROL AND DATA MANAGEMENT: Databasing for genetic samples). Documentation of genetic sample locations in cold-storage units should be as precise as possible so that samples can be located quickly (see INVENTORY CONTROL AND DATA MANAGEMENT: Sample labeling and tracking). Dates can be easily confused because their format differs throughout the world; thus, recorded dates should be formatted consistently and in an unambiguous manner. Security for electronic records should include password protection and automatic time-outs on computers and online databases, as well as scheduled backups for all data. Large collections should have electronic records backed up daily on a network or remote secure server, whereas small collections might consider doing local backups on a weekly basis.
Emergency procedures
Collections should have emergency procedures, including evacuation procedures and detailed disaster plans, outlined in their SOP to address how personnel should respond to various situations, ranging from laboratory incidents to natural disasters[18] [19]. Generally, emergency procedures and disaster preparedness should be developed to address incidents at various levels of involvement, including:
- Issues confined to the genetic collection (e.g., clean-up of chemical spills, transfer of genetic samples from a failed cold-storage unit)
- Building-wide or institution-wide events (e.g., flood or water damage as a result of plumbing issue or roofing leak)
- Local issues (e.g., city-wide power outage)
- Regional events (e.g., earthquake, hurricane, tornado, tsunami)
Because emergencies with genetic resources can become disasters if immediate action is not taken, it is recommended that a risk assessment is conducted and personnel have regular reviews and drills to ensure their familiarity with emergency procedures and backup plans for every conceivable situation (see FACILITY MANAGEMENT: Backup precautions). It is also essential that personnel are familiar with the locations of all equipment and tools needed to quickly and efficiently perform their responsibilities during each type of emergency, ranging from how and where to transfer samples from a failed unit to how to turn on backup power during a power outage. Contact information for personnel responsible in case of emergency in the order that they should be contacted, facilities managers, and outside contacts for emergencies (e.g., power companies, fuel supply companies, important contractors) should be included in the SOP document, provided to those responding to off-site alarms, and clearly posted in the collection. Contact information should be regularly reviewed to ensure that it remains current.
Genetic Sample Processing
Genetic samples require specialized storage to maintain their viability, but the manner by which they are initially preserved when collected and any subsequent changes made prior to their deposition in a collection also greatly affects their utility in research. In addition, procedures used by collection personnel to prepare the samples for deposition in long-term storage can have detrimental consequences if not completed properly.
Initial preservation procedures
The methods currently used to preserve genetic material during initial sampling vary widely owing to the sampling location, tissue type, and intended research use. A comprehensive treatise of methods to preserve genetic samples is discussed in Nagy (2010)[20]. Of all the methods examined, flash-freezing using liquid nitrogen or a mixture of dry ice and ethanol is considered to be the one of the best ways to preserve samples because the speed by which the sample is frozen prevents large ice crystals from forming and no preservative is needed, which maximizes the research potential of the sample. Some chemical agents or buffers (e.g., glycerol, dimethyl sulfoxide [DMSO]) are used to protect macromolecules and/or tissue integrity from damage caused by ice formation during cryopreservation techniques. Buffers, chemical preservatives, and alcohols, especially ethanol, do not require immediate refrigeration and are frequently used for the initial preservation of samples because it circumvents the complicated logistics involved with flash-freezing samples in the field or keeping them cold during transport. All preservation techniques have caveats to their use, however, and genetic resource collections must be fully aware of both the benefits and limitations to make informed decisions.

- Flash-frozen
- Preserved with ≥ 95% ethanol (zoological samples)
- Buffers and chemical preservatives
- - DMSO (in many different aqueous solutions; one of the most commonly used formulations is a salt-saturated solution of DMSO (20% DMSO, 0.25 M ethylenedi- aminetetraacetic acid [EDTA], sodium chloride [NaCl] saturated, pH 7.5[20])
- - RNAlater (Ambion, Austin, TX)
- - Allprotect Tissue Reagent
- - Lysis buffers
- Buccal swabs
- Whatman FTA (GE Healthcare Bio-Sciences, Pittsburgh, PA) filter paper
Desiccation methods, commonly used to preserve botanical samples, use either physical processes or chemical agents to dehydrate samples. These methods can be very effective in preserving samples if they are maintained in a humidity-controlled environment after the desiccation process. Physical processes that lead to desiccation include:
- Sun-drying
- Air-drying
- Flash-drying
- Oven-drying
- Vacuum-drying
- Freeze- drying
Substances that induce natural desiccation include:
- Rice
- Sodium chloride (NaCl)
- Calcium sulphate (CaSO4, commonly known as drierite[20])
- Sodium silicate (obtainable in powder, crystal or gel form).
Freeze-drying (lyophilization or cryodesiccation) is the controllable dehydration of samples by vacuum desiccation. This method involves the conversion of water within the sample into ice, crystallization of the sample, sublimation of ice under a vacuum, and subsequent evaporation of remaining water from the crystallized sample[21]. Silica gel beads are commonly used by botanical collectors as a desiccant with the advantage that whole samples can be stored at room temperature as long as the material is stored in tightly sealed containers and are regularly checked for dryness[22].
Chemical desiccation, which involves adding a chemical to extract moisture from samples, can be completed using a number of different substances, including:
- Amyl acetate
- Hexamethyl-disilazane
- Xylene (which is the chemical Dimethylbenzene),
- Methyl cellosolve/cellusolve (also known as ethylene glycol monomethyl ether)
- Calcium oxide (CaO, commonly called lime)
- Sulphuric acid (H2SO4)
Each of these chemical methods has certain considerations for the samples and personnel that should be closely examined before working with them[23]). Regardless of the method of desiccation, moisture content must be continuously controlled or samples quickly degrade. In addition, samples preserved in this manner are more sensitive to thermal decay at higher temperatures due to their reduced water content and should be stored in a low-temperature environment as soon as possible to ensure that samples remainviable.
Collection staff often does not have control of how genetic samples are originally preserved, and most genetic resource collections associated with natural history museums accept samples that are preserved using numerous different methods[2]. As more information is discovered about preservation methods themselves, it is becoming more important to know how samples were preserved and handled. Collection managers should make every effort to record the initial preservation methods used and any subsequent changes to storage for their samples, including media or containers. Both media and temperature can affect the ways that samples can be used for future molecular analysis; thus, all curation data for genetic samples should be made available to researchers before their selection and use. Research advancements are constant in molecular studies, and future technological developments might allow for the stabilization and storage of biological samples at room temperature, which could eventually eliminate the need for low-temperature storage environments for newly collected samples. To determine if these new emerging technologies will be effective for existing genetic collections, the detailed curation history regarding how each individual sample was preserved, stored, and utilized will become increasingly important.
Storage containers
Genetic resources can be stored in a variety of ways, depending on the tissue type, sample size, and cold-storage methods used in a collection. Primary storage containers of the samples themselves can include plastic bags, paper envelopes, reaction plates, or vials. When primary storage containers are accessioned into a collection, they must be examined to determine if they are appropriate for the type of cold storage being used in the collection. The SOP should clearly define acceptable storage containers and encourage their in-house researchers to use them because any variation could involve material and staff costs to rectify. For all types of cold storage, the most commonly used sizes of vials are between 1.2 and 2.0 ml, which is the size and configuration that maximizes storage capacity while retaining ease of handling [2].
One area of immense variability is with the number of vial types used in natural history collections [2]. Potential vial issues are the same for both mechanical freezers and cryovats, although more extreme for cryovats because of their colder temperatures and quicker temperature change. Samples stored using LN2 must have vials that are rated for use with cryogenic temperatures, which are most often made of polypropylene and include screw-top caps. Some additional useful information about vials include:

- Glass vials are not recommended because of their fragility when handling and vulnerability to cracking when stressed.
- Microcentrifuge vials with pop-off lids are not recommended because liquid nitrogen can enter them and cause them to open or explode.
- Self-standing vials (flat-bottom or skirted) may be useful to curatorial staff.
- Vials that allow for locking into a rack for one-handed operation may allow curatorial staff to process samples more quickly.
- Vials can have threads located internally or externally on the vial opening.
- - Externally-threaded closures promote more sterile conditions because internal threading can allow contaminants to enter if the cap is placed on an unclean surface when removed.
- - Externally-threaded vials can be susceptible to cracks and loss of air-tightness, which can lead to sample dessication or oxidation [24][25].
- - Internally-threaded vials might allow increased storage capacity, depending on the vial selected, but users also suggest that material can be trapped within the threads of this vial type[26].
- Some manufacturers suggest that vial caps that incorporate a silicone gasket or O-ring (internally or externally threaded) are ideal for vapor-phase LN2 freezing because the seal is enhanced, but care must be taken if the vial cap is over-tightened because the gasket can become distended. In addition, the presence of gaskets or O-ring might improve the initial performance of seals but can be problematic when used with some alcohols (e.g., ethanol) because some gasket material, such as silicone, is vapor permeable.
- Vial manufacturers recommend that samples not be immersed in LN2 unless they have secondary containment because the accidental entrapment of liquefied nitrogen inside the vial leads to pressure build up and, upon removal, rapid vaporization of the liquid can result in leakage or even explosion (see HEALTH AND SAFETY: Liquid nitrogen safety). Heat-sealing vials into flexible polyethylene tubing is recommended for safe storage in the liquid-phase environment.
Depending on the size of the samples and their primary storage method in the collection, various secondary and tertiary storage containers (e.g., boxes, cassettes, sample storage canes for immersion in LN2, racks) can be used to organize samples and maximize space. The majority of natural history museums recently surveyed organizes their collections with a vial box and rack system[2]. The box-and-rack system is a simple but effective way to maximize space within a cold-storage unit and reduce the amount of time needed to search for a specific box. The overall cost of box-and-rack systems depends on the style and number of both the boxes and racks purchased. The use of racks also decreases potential risks to the collection when personnel are retrieving samples. Collections without racks often stack boxes on top of one another within cold-storage units, forcing personnel to remove or displace boxes to access those underneath or behind. In addition, the movement of individual boxes to retrieve samples requires more time, increases the possibility that samples will thaw, and decreases the chance that boxes will be put back in their original location. Lastly, racks allow samples to be quickly moved to other freezers in the event of a freezer failure and decrease the possibility that samples are misplaced while in a temporary storage location.
Racks systems made from aluminum or stainless steel can house most standard-sized boxes and can be oriented horizontally or vertically to fit in mechanical upright or chest freezers, as well as LN2 cryovats. Aluminum might be chosen for racks in collections that need precise and controlled freezing of samples because this metal is a better energy conductor than stainless steel. Stainless steel racks are more durable and, because the steel does not oxidize, they remain clean. Racks most often come with a locking rod that runs through the front of the shelves, ensuring that boxes are held in place when the rack is moved. Racks also can have spring clips instead of locking rods, which allow quicker access to boxes, but can be problematic if the racks are bumped or dropped. Identifiers can be added by riveting or etching onto racks, or by labels (e.g., unique locating identifiers, barcodes) that can be affixed to the tops of racks and rack shelves (see INVENTORY CONTROL AND DATA MANAGEMENT: Sample labeling and tracking).
A number of different types of vial storage boxes can be used, such as cardboard, chipboard (paperboard), fiberboard, metal, polycarbonate, or polypropylene. It is recommended that moisture-proof boxes be used even though they are more costly, because water repellency increases their long-term durability. When purchasing new boxes, care should be taken to ensure that they are compatible with both the existing rack system and the cold-storage equipment. Collection managers should be aware that polypropylene boxes with hinged lids, which are often used in the field because they are shatter-resistant and have attached lids, might not fit in standard-sized racks. In addition, personnel in collections using either the liquid or vapor phase of nitrogen should use boxes with holes or slots present on the underside of the box to allow the LN2 to drain. Collections using cryovats should confirm that particles of cardboard, chipboard (paperboard), or fiberboard will not prevent equipment from functioning properly if boxes begin to degrade; otherwise, a more durable type of box should be used. Aspects of ordinary use are another important consideration for storage boxes in a collection. Collection managers should be aware that boxes that have numbered, gridded inserts inside might be difficult to read after being removed from cold temperatures because of frost. In contrast, boxes with grid numbering present on the lid, rather than the box itself, can have frost easily wiped off; however, finding the correct vial may be difficult once the lid is removed because care must be taken to keep the lid numbering aligned with the internal grid.
Sample transfer
When samples are received by collection staff, they might need to be transferred into new primary storage containers, especially if they are stored in a manner that is incompatible with the cold-storage system or if initially preserved in sub-optimal conditions for long-term storage (e.g., preservatives need to be removed). Collection personnel should ensure that contact between different specimens is avoided and all instruments used in the tissue transfer process are handled in such a way that ensures that biological contaminants are destroyed. Disposable equipment (e.g., single-use blades, disposable forceps) replaced after on use greatly reduces the chances of sample contamination, but this practice can become too costly for many collections. Several methods (e.g., heat/flame, chemical agents, steam sterilization in an autoclave) can be used to prevent contamination between genetic samples, but collection managers must be sure that their particular procedures denature or destroy all contaminating genetic material. Some practices, such as cleaning instruments using detergent and water, render instruments and surfaces safe to touch, but these methods do not protect samples from cross-contamination. Disinfection of work surfaces, decontamination of equipment, and sterilization procedures are all needed to ensure safe operations for both staff and genetic samples, and these techniques can vary depending on the task at hand.
Comprehensive procedures should clearly outline which handling methods are appropriate for the various tasks when working with samples. Some techniques, such as autoclaving and use of UV light, destroy all biological matter but require a longer time to accomplish, and thus are better utilized before and after processing a batch of samples. Alternatively, other methods, such as heat/flame or hydrogen peroxide, could be used to immediately decontaminate subsampling tools and ensure no cross-contamination while working through a batch of samples, because ease and speed of use is important. If a chemical agent such as hydrogen peroxide or bleach is used to clean equipment or surfaces, procedures should ensure that those agents do not contaminate samples because these techniques destroy biological matter (e.g., dry instruments thoroughly before manipulating samples). Personnel should also be careful not to inadvertently contaminate the samples by touching their own body or clothes, or allowing hair to come in contact with samples. In addition, they should always wear the proper PPE to protect genetic samples and for their own personal safety (see HEALTH AND SAFETY: Personal protective equipment).
Inventory Control and Data Management
The ability to find a specimen is essential for the curation of any natural history collection. The manner by which the physical locations of genetic samples are tracked is particularly important in their curation because it is virtually impossible for personnel to search the entire collection if a particular sample is missing. In addition, proper inventory and data management allows collection managers to maximize the capacity of their cold- storage units while reducing the amount of time needed to locate samples, which is crucial given that the quality of some genetic material can be reduced with each freeze–thaw event.
Sample labeling and tracking
Proper sample tracking is key to ensuring that cold-storage equipment does not have to remain open for long periods, or samples are not repeatedly exposed to temperatures that initiate thawing. An appropriate tracking system could include:
- Sample labeling
- Multiple levels of container labeling
- Use of a database to record sample location data
- Using a convention for numbering that assigns unique locating identifiers (e.g., barcodes) to all levels of sample storage (e.g., primary, secondary, and tertiary containers)
It is recommended that for maximum efficiency, sample vials stored within LN2 cryovats or mechanical freezers should have unique locating identifiers assigned to the cryogenic vials, as well as unique locating identifiers assigned to the associated boxes, shelves within racks, racks in their entirety, and individual cold-storage units. Each sample vial can then be located in the collection by a unique location number combination. Any labels placed on vials or storage containers should be typewritten or computer-generated; hand-written identifiers might be difficult to read due to the handwriting or decomposition of the ink as a result of cold temperatures or mechanical friction. Upon arrival to a collection, samples might need further curation to meet collection standards, including the addition of typewritten or computer-generated labels to vials or the transfer of samples into the appropriate type of vials. Extreme care must be taken because most genetic samples are initially labeled using reference numbers written on the vial by the researcher. All label placements should be tested under projected environmental conditions to ensure that ink, adhesive, and the label itself withstands the cold-storage temperatures. On secondary containers, such as boxes or racks, labels should be placed in areas where friction is minimal to reduce the risk that the label face is worn down by repeated scratching or rubbing.
Barcodes labels rated for cryogenic conditions or vials manufactured with barcodes are commonly used by genetic resource collections to facilitate sample tracking, including for primary and other hierarchies of containers [2]. Preprinted or self-printed barcode labels that are mostly transparentand wrap completely around vials, allow information hand-written on the vials to be viewed when positioned over the writing. Vials manufactured with barcodes on the side or bottom are less commonly used, most likely because these vials rarely have an area where researchers can include hand-written information. Barcodes inserted into vial caps do facilitate he barcoding process because they require less handling time when compared to vial-wrapping labels, but there are added risks that inserts could fall out or a cap could become disassociated from the vial itself. Radio frequency identification (RFID) tags transmit unique locating identifiers associated with tagged objects and, unlike traditional barcodes, these tags do not need to be within the line of sight of the reader. RFID technology is currently being used only to track secondary and tertiary containers (e.g., boxes, racks) within the natural history community, but this method could potentially be used to track primary containers when the tag size and associated costs decrease [2].
Databasing for genetic samples
By their nature, genetic resource collections generate and track a large amount of data associated with their samples. A computer-based inventory system, such as a stand-alone database, internal spreadsheet, or networked database, is essential so that all sample metadata can be tracked[27]. The system should have the capacity to assign a unique identifier to each genetic sample entered in the database and associate all derived genetic samplings and derivatives with the original specimen, which might be the original genetic sample itself or a traditional voucher specimen. It is essential that a tissue sample or genetic extract can be readily linked to the traditional voucher specimen. Changes/updates to data, including taxonomic identification, should be made to all preparation types, even if data are tracked separately for the traditional voucher specimen and genetic sample, The chosen database should accommodate for museum-wide variables given that traditional voucher specimens are likely housed apart from their associated genetic samples due to their different storage and conservation needs and, in addition, personnel curating these two collections are likely different. Regardless of the chosen database, data standards are also critical to ensure that the format of the information, syntax and punctuation are consistent, allowing databases to function as research and curation tools when used in basic queries, enhances the exchange of data among research and informatics partners, and facilitates the utilization of data with data aggregators (e.g., Global Biodiversity Information Facility [GBIF], iDigBio, VertNet).
Those curating genetic resource collections associated with natural history museums are currently using a number of different platforms to track data, including[2]:
- Free-access database application systems developed for museums (e.g., Arctos, Specify)
- Commercial database application systems (e.g., FileMaker Pro, Microsoft Access, FreezerPro)
- Web delivery through data aggregators (e.g., GBIF, HerpNET, ORNIS)
- Internally written applications
All of the systems currently being used have benefits and drawbacks; before selecting a system, collection managers should evaluate the size of their genetic resource collection and internal computing resources, and determine how to integrate o link data associated with genetic samples and traditional voucher specimens. Free database application systems developed for natural history collections can easily associate specimen parts, but these systems might need to be customized to include data fields specific to genetic samples, such as changes to preservation, freeze–thaw events, and remaining volume. Some commercial systems (e.g., KE EMu) can accommodate genetic sample data, but some collection managers might find annual license fees too costly to maintain. Also, some specialized systems (e.g., FreezerProH) can prioritize sample location data, which is important for a larger genetic collection, but disassociates traditional voucher specimen data from genetic samples. The use of a web-based data aggregator (e.g., Global Genome Biodiversity Network [GGBN[28]], GBIF) can allow external users to access data, but an internal platform is still necessary to allow collection personnel to track genetic sample metadata. Internally written applications might seem ideal because they can be tailored, but they require personnel dedicated to their development and maintenance, and who have an understanding of how to build the system with the flexibility and scalability needed for data and metadata growth.
Use of Collections
Most natural history museums have active loan/gift programs, but the consumptive nature of genetic resources requires collections to develop specific policies to address the demand on this unique type of collection. Genetic collections must also ensure that the manner by which genetic samples are processed and transported preserves the integrity of the original sample and all subsequent subsamples.
Loan policies
In the context of natural history museums, a loan is a temporary transfer of a single specimen or lot of specimens, generally for research, for a specified period of time. Most loan policies for traditional natural history specimens are applicable to genetic samples but, owing to the consumptive nature of this resource and unique issues related to custodianship, clear policies should be developed in relation to the distribution of genetic samples. Baker and Hafner (1984) suggested that the term ‘‘loan’’ be replaced with ‘‘gift’’ or ‘‘donation’’ when discussing transfer of genetic samples between collections and researchers because the specimens are not returned; however, Zimkus and Ford (2014)[2] found that some genetic collections do request unused samples to be sent back. Loan/gift policies should be explicit how custodianship issues, as well as permissions to approve the transfer of genetic material, are made, especially for institutions with a centralized repository. Unlike traditional natural history specimens within an institution, genetic samples might be part of a voucher specimen that was accessioned by another collection before the sample itself was deposited in the genetic collection.
Because genetic collections are consumptive, loan/gift policies should clearly outline the required information that should be submitted in sample requests to justify that a material transfer is warranted. The following information is recommended for inclusion in loan/gift requests:
- Objectives of the proposed research and its scientific merit
- Taxa and total number of genetic samples requested
- Experimental protocol to be employed
- Amount of genetic material requested per sample
- Desired method of transport (e.g., room temperature in preservative, frozen on dry ice)
- Plans for the dissemination of knowledge gained from the proposed research with the originating institution and scientific community, including:
- - Publications resulting from use of the samples
- - Online publication of sequence data
Loan/gift policies should also clearly state the allowable use of genetic samples and associated metadata. Policies should stipulate that loans/gifts may not be transferred from one institution to another without the written permission of the originating institution. This also ensures that those receiving samples do not patent or otherwise profit from the use of specimens (as outlined in the Convention on Biological Diversity). Researchers might also be obliged to acknowledge the institution in all publications resulting from use of their loan/ gift material and make available citations or reprints of such publications.
Loan/gift policies for genetic resources differ from those of other types of natural history specimens because genetic sequence data is generated from their consumptive use. The majority of genetic resource collections surveyed request that researchers submit genetic sequence data to a public genetic sequence database, such as NCBI GenBank (http://www.ncbi.nlm.nih.gov/)[2]. This requirement is important for consumable collections because it ensures that sequence data is available to other researchers, unnecessary work is not duplicated, and originating institutions comply with granting agreements to make data accessible. Whenever possible, collections should link the end products of research (e.g., genetic sequences) captured in communal databases to the original genetic samples and/or voucher specimen records found in the originating institution’s database. To ensure compliance, it is recommended that collection managers should follow up with researchers annually and consider loans/gifts ‘‘closed’’ only when all policy requirements are met.
If the institution provides the appropriate amount of material, the genetic samples loaned/gifted should be completely consumed by the researcher (see USE OF COLLECTIONS: Aliquoting Samples). If a portion of a genetic sample remains unused after the project, however, researchers might be unclear about what to do with the remaining samples. In a recent collection survey, institutions requested that researchers address leftover samples in various ways, including destroying the remaining samples, returning samples to the originating institution for destruction or reuse, or accessioning samples into the researcher’s personal or institutional collection [2]. The loan/gift policy should clearly outline the requirements of researchers in regards to any unused genetic material. It is recommended that subsamples that are returned to loaning collections for potential future reuse be maintained separately from the original samples in case the returning sample’s integrity was compromised (e.g., contaminated, mislabeled, improperly stored) while on loan. The use history of each sample is important to track, especially for returned material, because this allows personnel to inventory and use only returned samples if all other portions have been consumed (see [[#Databasing for genetic samples|INVENTORY CONTROL AND DATA MANAGEMENT: Databasing for genetic samples). When returned samples are reused, tracking also allows collection manager to inform researchers of the chain of custody of the returned sample, so that future researchers can evaluate the risks of use of such samples.
Aliquoting samples
To maximize their use and research potential, genetic resources should not be sent in their entirety; rather genetic samples should be aliquoted for internal or external use (see USE OF COLLECTIONS: Loan policies). Regardless of the end user, subsampling methods should be employed that maximize collection utility by minimally handling samples, effectively removing the smallest sampling amount, and reducing freeze–thaw events while manipulating samples. Implementing efficient organizational methods, from storage containers to database management systems, minimizes the amount of time required to locate samples. At any one time, only a manageable number of samples should be retrieved, so that cold-storage units do not remain open and the time that storage containers are kept outside of these units is minimized. During the subsampling process, samples should be kept as close to their normal storage temperature as possible. Depending on the temperature from which the samples were taken, liquid nitrogen, dry ice, or wet ice can be used to help keep samples cold during processing.
The amount of a genetic sample provided to a researcher should be scaled to their individual request to ensure long-term availability of the original sample for other researchers. The SOP should provide baseline standards to guide the amount of genetic material sent as a loan/gift, including considerations for the type of preparation requested (e.g., tissue subsample, aliquot of extraction, PCR product) and the experimental protocol to be implemented. In a recent collection survey, collections were found to set these sampling criteria in various ways [2]. Over one-third of the surveyed collections provided the approximate amount of tissue needed for two to three DNA extractions; fewer collections quantified the amount of a sample sent (i.e., ranging from 1 mm² to 6 mm² in size, weighing from 10 mg to 2 g), likely because measuring or weighing individual samples is a time-consuming process that most collections cannot afford. Collection managers should also consider whether to extract DNA, rather than send tissue samples, especially when rare samples or those with low remaining volumes are requested. Regardless of the general criteria, personnel working with genetic samples should be knowledgeable of the sample amounts needed for methods commonly conducted (e.g., DNA extraction, RNA extraction, PCR, cloning).
Packaging and shipping loans/gifts
As with traditional natural history specimens, loan/gift shipments of genetic samples should include loan paperwork on institutional letterhead that documents the contents, handling requirements, and policies of use (see USE OF COLLECTIONS: Loan policies). Before any loans/gifts are processed, collection personnel must:
- Determine all the national or international laws and regulations pertaining to the genetic samples and the shipment
- Include copies of all permits and certificates with the shipment in a location that is easily accessible on the outside of the package
- Include invoice that can be signed and returned by the researcher upon receipt of the samples
- Determine if special permits or requirements are necessary, including:[29]
- - US Department of Agriculture (USDA)
- - International Treaty on Plant Genetic Resources for Food and Agriculture (PGRFA)[30]
- - Convention on International Trade in Endangered Species of Wild Fauna and Flora (CITES)[31] [32], and various US domestic laws, including the Endangered Species Act (ESA)[33]
- - Lacey Act[33]
- - Migratory Bird Treaty Act (MBTA)
As the legal landscape evolves, collection personnel must receive the appropriate training, with applicable updates, in both national and international regulations, including the shipment of biological samples and dangerous goods (e.g., DOT, International Air Transport Association [IATA] Special Provision A180), and the recent ratification of the Convention on Biological Diversity Nagoya Protocol on Access and Benefit-Sharing. See Shipping and Handling of Dangerous Goods for additional information.
Loans/gifts of genetic samples can be shipped using various methods and, depending on the sample type and ultimate use, material transfers might require special means of shipping to preserve specimen integrity and quality. Cold or frozen material should be shipped in a manner that will maintain the appropriate temperature for the duration of the shipment with allowance for delay in arrival time. Refrigerant should last an additional 24−72 hours, depending on whether the shipment is domestic or international, especially because customs will be involved for the latter[17]. It is advised that refrigerated or frozen shipments are not sent on days that require transit over a weekend or holiday period, so as to avoid delays and ensure that recipients are available for immediate receipt of the samples. The coordination of shipping and receiving samples is important for all parties, so to avoid mishaps, both the shipper and recipient should track the package while in transit. Collection personnel should contact the recipient before sending the shipment to confirm that they are present to receive the package as scheduled and, again, contact the researcher to notify them when the shipment is specifically scheduled to arrive.
When packing, genetic samples should be positioned in the package so that they are surrounded by refrigerant on all sides, rather than having samples placed on top of or underneath refrigerant. Any empty space between samples and refrigerant should be filled with dunnage material (e.g., loosefill non-biodegradable peanuts, padding material). Specimens that are sensitive to humidity (e.g., botanical samples) should be shipped in sealed bags with desiccant to ensure that humidity levels are controlled in transit. The following are typical temperature conditions required for shipment of genetic samples, including the insulation and/or refrigerant that can be used to maintain the desired temperature (modified[17]).
- Ambient (20°–30°C): insulated packaging with a minimum of 4-cm-thick walls to protect from fluctuations in ambient temperature; chemical preservative might or might not be necessary, depending on sample type.
- Refrigerated (2°–8°C): insulated packaging with a minimum of 4-cm-thick walls with wet ice or gel packs; chemical preservative might or might not be necessary, depending on sample type.
- Frozen (-20°C): insulated packaging with a minimum of 4-cm-thick walls with gel packs designed for frozen temperatures.
- Frozen (-70°C): insulated packaging with a minimum of 4-cm-thick walls with dry ice pellets, sheets, or blocks. Note: dry ice (solid CO2) is considered a hazardous material.
- Frozen (at or below -150°C): LN2 dry shipper. Dry nitrogen shippers are insulated containers that contain LN2 that is fully absorbed in a porous material within the walls and, therefore, considered a non-dangerous product by DOT and IATA regulations.
Recently surveyed genetic resource collections were found to most frequently ship samples frozen using dry ice, or at ambient temperature using ethanol or DMSO as a preservative.[2] Shipping methods among collections likely differed due to overall cost, shipping restrictions, ease of shipment, and the intended use of the samples. With increasing regulations on shipments and shipping training for personnel, expenses have become prohibitive for many institutions and, as a result, many collections are either requesting or requiring that researchers offset the associated costs.
Health & Safety
Health and safety policies are essential because they protect personnel who are working with genetic resource collections, but these policies also ultimately protect the collection itself because they promote proper and efficient practices. All health and safety policies should be reviewed with the appropriate health and safety group at the institution and fully outlined in the SOP of the genetic collection.
General laboratory practices
Good laboratory practices should be implemented in genetic resource collections to protect staff from exposure to various hazards (e.g., potential pathogens, chemicals, sharps). For staff safety, certain activities should be prohibited in the laboratory or collection space, including:
- Eating
- Drinking
- Storing food
- Smoking
- Applying cosmetics
- Handling contact lenses
- Mouth pipetting
For collections harvesting genetic samples from traditional voucher specimens, collection managers must ensure that any biosafety waste is processed in accordance with institutional regulations and any pertinent local, state, or national guidelines. Policies should be instituted for the safe handling and disposal of sharps (e.g., needles, razor blades, scalpels). Lastly, good laboratory practice includes washing hands at the end of preparation work, after gloves are removed, and prior to leaving the laboratory.
Personal protective equipment
All personnel, including visitors, should wear appropriate and approved clothing (e.g., buttoned lab coats, long pants, shoes that completely cover the feet) when working in a laboratory environment, such as a genetic collection.[34] Shorts, skirts and open-toe shoes are not appropriate, especially in labs that require a Biosafety Level 2 designation. In addition, long hair and dangling jewelry should be secured. Depending on the laboratory application, personnel should wear the appropriate gloves; this includes latex or nitrile gloves when handling chemicals or biological samples, cryogenic gloves to protect against frostbite when working with ultracold equipment or samples, and heat-resistant gloves when using autoclaves or other equipment that reach high temperatures. Eyes should always be protected from exposure to chemicals and biohazards by using safety glasses, goggles or face shields; eye and face protection devices should comply with American National Standards Institute recommendations (i.e., ANSI Z87.1) when used with chemicals.
Liquid nitrogen safety
Those collections that use LN2 storage equipment require additional safety precautions and equipment specifically rated for cryogenic conditions. Specialized ventilation and oxygen monitors might be needed to protect personnel from the risk of oxygen depletion and possible asphyxiation (see FACILITY MANAGEMENT: Ventilation; FACILITY MANAGEMENT: Oxygen monitors). When working with LN2, appropriate PPE is recommended:
- Cryogenic gloves, which are water-resistant insulated gloves rated for cryogenic temperatures, to protect the hands from cold temperatures and nitrogen vapor
- Cryogenic aprons to protect the body when using the liquid phase of nitrogen
- Eye protection (e.g., safety glasses) when working with samples that have been stored in the liquid phase of nitrogen because sample vials can burst without warning if LN2 enters them through minute cracks
- Goggles and/or a face shield when dispensing LN2 to additionally protect the face and eyes from possible splashing
- Closed-toe shoes (not canvas) that can be quickly removed (e.g., few laces, buckles, zippers)
- Lab coats
- Pants without cuffs; pants should not be tucked into shoes or boots because LN2 can become trapped if spilled
If nitrogen in the liquid form contacts the skin or eyes, the tissue should be immediately flooded or soaked with tepid or warm water (105°F –115°F [41°C–46°C]). Hot water (above 46°C) should never be used because this can cause additional damage to the skin. In addition, the skin must not be rubbed because this can damage the tissue; thus, any contact should involve only gentle patting or dabbing. If LN2 comes in contact with the eyes, contact lenses should be removed immediately and the eyes flushed with tepid or warm water for at least 15 minutes, and the upper and lower eyelids should be lifted occasionally during the flushing process. If any injury occurs from a cryogenic burn, medical attention should be sought as soon as possible.
Cryogenic fluids must be handled and stored only in containers specifically designed for these products. Unapproved materials can become brittle and shatter or become over-pressurized, causing risks of explosion. All cryogenic vessels must be equipped with pressure-relief devices (e.g., relief valve, venting lid/stopper) to prevent excessive pressure build-up. A tremendous amount of force can be generated if liquid nitrogen rapidly vaporizes, so pressure-relief devices on LN2 equipment should be monitored to ensure that they are functioning properly. Transfer operations involving open cryogenic containers, such as dewars, should be conducted slowly to minimize boiling, splashing, and thermal shock to the receiving vessel. A phase separator (i.e., fitting that attaches to end of a transfer hose that separates gas from liquid)can also be used to control the vapor path while dispensing. When dispensing or pouring LN2, receiving vessels should be placed as close as possible to the source; a table or other sturdy surface can be used to position the vessel in the proper location. Funnels should not be used to channel LN2 because they can freeze, creating a splash hazard, or be propelled upwards if the container is overfilled.
Dry ice safety
Use of dry ice (i.e., solid phase of CO2) is regulated and requires specialized training for use in shipments. When dry ice is used, collection managers should ensure that there is adequate ventilation because CO2 can displace oxygen, causing loss of consciousness or even asphyxiation. All confined areas should be closely monitored when dry ice is in use. Walk-in freezers should be kept free of dry ice because carbon dioxide can rapidly build up without regular air exchange; owing to this inherent danger, proper signage should be posted outside walk-in freezers to prevent staff from placing dry ice into walk-in freezers.
Biosafety
Collection managers should consult all federal biosafety and biocontainment regulations relevant to the activities conducted that involve potentially hazardous biological materials within the collection. Policies should incorporate all regulations hat outline standard and special practices, safety equipment, and facility requirements to minimize potential hazards to laboratory personnel and the environment. USDA permits could be needed for work with some specific taxa, such as birds, some mammals, and plants. Depending on the biosafety level required for the collection as determined by the USDA, certain requirements might need to be met, including:
- Training in handling pathogenic agents
- Restrictions to collection access when work is being conducted
- Conduction of particular work in a biological safety cabinet
A biosafety cabinet (BSC), also known as a biological or microbiological safety cabinet, is an enclosed, ventilated workspace for handling materials potentially contaminated with pathogens (e.g., Exotic Newcastle Disease, Foot-and-Mouth Disease, Hantavirus, Highly Pathogenic Avian Influenza). BSCs differ from fume hoods because BSC exhaust air is HEPA-filtered as it exits. BSCs are classified as one of three classes by their level of protection provided to personnel and the environment (i.e., Class I, II, III). Class II Type A2 BSC, which includes a minimum inflow velocity of 100 ft/min (30.5 m/min), is the most commonly used BSC providing protection for personnel, the environment, and the samples. Collection managers should be aware that gas lines should not be installed into BSCs because air is contained within, rather than being exhausted from the cabinet, leading to the potential build up of flammable materials. Additionally, open flames, such as those generated by Bunsen burners, can detrimentally affect airflow in a BSC, disrupting the pattern of HEPA-filtered air supplied to the work surface. To provide adequate protection, BSCs require proper use, monitoring, and regular maintenance. SOP documents must outline these approved activities, including appropriate height of the sash opening to minimize airflow, methods used to decontaminate surfaces, as well as testing and certification protocols for the unit itself (see OPERATIONAL BEST PRACTICE: Equipment preventative maintenance, repair, and replacement).
Chemical safety
Genetic resource collections should maintain an inventory of all chemicals used and access to Safety Data Sheets (SDS) for every chemical used within the collection. A chemical hygiene plan should also be included in SOP documents, which outlines the appropriate use of chemicals in the collection, as well as their containment and procedures for clean-up if spills occur. Personnel should have the appropriate training for all procedures related to chemical safety, which frequently involves training by institutional groups, such as health and safety and the fire group (see OPERATIONAL BEST PRACTICE: Training).
Fire safety
Collection personnel must comply with all local fire and building codes. Automatic fire detection units and suppression systems, including appropriate hand-held fire extinguishers and sprinkler systems, are recommended. The SOP should include information regarding major fire hazards and potential ignition sources, as well as what working materials are flammable hazards (e.g., ethanol). Personnel should be trained in fire prevention and emergency procedures relating to evacuation if a fire occurs (see OPERATIONAL BEST PRACTICE: Training). All fire detection systems and suppression systems should be tested on a regular basis and frequently involve health and safety, fire, and building facility personnel at the institution (see OPERATIONAL BEST PRACTICE: Equipment preventative maintenance, repair, and replacement).
Ethical and Legal Best Practice
The accumulation and use of genetic samples involve numerous ethical and legal issues. Most natural history museums have institutional policies that address legal compliance and ethical standards, but many times, genetic samples are present in individual laboratories or stand-alone collections whose activities might not be specifically addressed in the broader institutional policies. In these instances, dedicated policies might not be in place to govern broad aspects of legal and ethical issues associated with the initial collection, transport, and use of genetic samples. Genetic resource collections are subject to the same regulations, laws, and consequences as traditional natural history collections. As such, they must have accessioning practices that ensure and document that all samples are legally collected, transported, and acquired by the collection. Copies of all necessary permits, including collecting permits, relevant Material Transfer Agreements, export permits from the country of origin, and import permits into the country of the genetic collection, must be on file within the institution or genetic resource collection. The accession process should also ensure and document that all animals collected were done so in a manner consistent with pertinent guidelines, such as Institutional Animal Care and Use Committee (IACUC) regulations.
Unlike most traditional natural history collections, genetic resource collections make samples available to researchers for molecular analyses with the understanding that derivatives and even possible genetic modifications of the original sample will be produced. It is a legal responsibility that collections personnel, therefore, act as custodians to ensure that genetic samples are used in accordance with all laws and governing policies,including the original collecting or acquisition agreements and pertinent international conventions[35] [33]. Collection managers should be aware that countries or other governing entities might have restrictions in relation to the commercial use of genetic samples, whereas educational or research use is permitted. In addition, entities that retain ownership (e.g., US National Park Service) can have specific regulations in relation to exportation, importation, or use of samples.
To document compliance and provide responsible stewardship for consumptive genetic resources, collection personnel should track the use history of all genetic samples and their derivatives, and link this information to the available metadata (e.g., NCBI GenBank; see INVENTORY CONTROL AND DATA MANAGEMENT: Databasing for genetic samples). Loan/gift policy must, therefore, be explicit in the approved uses of genetic samples and associated metadata, as well as expectations for what the researcher should do with any samples remaining after the completion of the research (see USE OF COLLECTIONS: Loan policies). Policy should also clearly outline requirements resulting from use of the genetic material. Research users and collection managers should both make a dedicated effort to ensure that collections are formally acknowledged for use of their samples and collections are notified of published studies that result from the use of their material. Knowledge of sample use is ital to genetic resource collections, because they must justify their significance in research to both their institution and outside funding bodies. Lastly, copyright and intellectual property rights in relation to genetic sample metadata provided to researchers or presented on public websites should be accompanied by policy that outlines the terms and conditions of its use, including the requirements to share results from the research.
Contributors
Breda Zimkus, Linda S. Ford
Source Material
Zimkus, B.M. and L.S. Ford. 2014. Best Practices for Genetic Resources Associated with Natural History Collections Recommendations for Practical Implementation![]() . Collection Forum 28(1-2), pp. 77-112.
. Collection Forum 28(1-2), pp. 77-112.
Links
- DNA Banks and Genetic Resources Repositories in the United States
- International Society for Biological and Environmental Repositories
- The Global Genome Biodiversity Network
- The Nagoya Protocol on Access to Genetic Resources and the Fair and Equitable Sharing of Benefits Arising from their Utilization (ABS) to the Convention on Biological Diversity
References
- ↑ Wieczorek, J., D. Bloom, R. Guralnick, S. Blum, M. Doring, R. Gionvanni, T. Robertson, and D. Vieglais. 2012. Darwin core: An evolving community-developed biodiversity data standard. PLoS ONE 7(1): e29715.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 Zimkus, B.M. and L.S. Ford. 2014. Genetic resource collections associated with natural history museums: A survey and analysis to establish a benchmark of standards. Pp. 9–44 in DNA Banking for the 21st Century. Proceedings of the U.S. Workshop on DNA Banking (W.L. Applequist and L. Campbell, eds.). William L. Brown Center, St. Louis, Missouri. 187 pp.
- ↑ Savolainen, V., M.P. Powell, K. Davies, A. Corthals, and G. Reeves (eds). 2006. DNA and Tissue Banking for Biodiversity and Conservation: Theory, Practice and Uses. Kew Publishing, Royal Botanic Garden, Kew, England. 151 pp.
- ↑ Hanner, R., A. Corthals, and H.C. Dessauer. 2005. Salvage of genetically valuable tissues following a freezer failure. Molecular Phylogenetics and Evolution 34:452–455.
- ↑ International Society for Biological and Environmental Repositories. 2012. 2012 Best practices for repositories: Collection, storage, retrieval, and distribution of biological materials for research. Biopreservation and Biobanking 10:79–161.
- ↑ Engstrom, M.D., R.W. Murphy, and O. Haddrath. 1990. Sampling vertebrate collections for molecular research: Practice and policies. Pp. 315–330 in Managing the Modern Herbarium (D.A. Metsger and S.C. Byers, eds.). Granville Island Publising, Vancouver, Canada. 384 pp.
- ↑ Karlsson, J.O. and M. Toner. 1996. Long-term storage of tissues by cryopreservation: Critical issues. Biomaterials 17:243–256.
- ↑ Kilpatrick, C.W. 2002. Noncryogenic preservation of mammalian tissues for DNA extraction: An assessment of storage methods. Biochemical Genetics 40:53–62.
- ↑ Mutter, G.L., D. Zahrieh, C. Liu, D. Neuberg, D. Finkelstein, H.E. Baker, and J.A. Warrington. 2004. Comparison of frozen and RNALater solid tissue storage methods for use in RNA expression microarrays. BMC Genomics 5:88.
- ↑ Corthals, A. and R. DeSalle. 2005. An application of tissue and DNA banking for genomics and conservation: The Ambrose Monell Cryo-Collection (AMCC). Systematic Biology 54:819–823.
- ↑ Gemeinholzer, B., I. Rey, K. Weising, M. Grundmann, A.N. Müllner, H. Zetsche, G. Droege, O. Seberg, G. Petersen, D.M. Rawson, and L.A. Weigt. 2010. Chapter 7—Organizing specimen and tissue preservation techniques in the field for subsequent molecular analyses. Pp. 129–157 in Manual on Field Recording Techniques and Protocols for All Taxa Biodiversity Inventories (J. Eymann, J. Degreef, C. Ha¨ user, J.C. Monje, Y. Samyn, and D. VandenSpiegel, eds.). Belgian National Focal Point to the Global Taxonomy Initiative, Brussels, Belgium. 653 pp.
- ↑ Nagy, Z.T. 2010. A hands-on overview of tissue preservation methods for molecular genetic analyses. Organisms Diversity & Evolution 10:91–105.
- ↑ Buś, M. and M. Allen. 2014. Collecting and preserving biological samples from challenging environments for DNA analysis. Biopreservation and Biobanking 12:17–22.
- ↑ Clark, G.N. 1999. Sperm cryopreservation: Is there a significant risk of cross-contamination. Human Reproduction 14:2941–2943.
- ↑ Hanner, R., A. Corthals, and H.C. Dessauer. 2005. Salvage of genetically valuable tissues following a freezer failure. Molecular Phylogenetics and Evolution 34:452–455.
- ↑ Savolainen, V., M.P. Powell, K. Davies, A. Corthals, and G. Reeves (eds). 2006. DNA and Tissue Banking for Biodiversity and Conservation: Theory, Practice and Uses. Kew Publishing, Royal Botanic Garden, Kew, England. 151 pp.
- ↑ 17.0 17.1 17.2 [ISBER] International Society for Biological and Environmental Repositories. 2012. 2012 Best practices for repositories: Collection, storage, retrieval, and distribution of biological materials for research. Biopreservation and Biobanking 10:79–161.
- ↑ [ICOM] International Council of Museums. 1993. Guidelines for Disaster Preparedness in Museums. http://icom.museum/fileadmin/user_upload/pdf/Guidelines/guidelinesdisasters_eng.pdf (1 January 2014). (Off-print from Museums Security and Protection: A Handbook for Cultural Heritage Institutions [D. Listen, ed.] ICOM in conjunction with Routledge, London, New York. 319 pp.)
- ↑ Dorge, V. and S.L. Jones. 1999. Building an Emergency Plan: A Guide for Museums and Other Cultural Institutions. Getty Conservation Institute, Los Angeles. 272 pp.
- ↑ 20.0 20.1 20.2 Nagy, Z.T. 2010. A hands-on overview of tissue preservation methods for molecular genetic analyses. Organisms Diversity & Evolution 10:91–105.
- ↑ Adams, G. 2007. The principles of freeze-drying. Methods in Molecular Biology 368:15–38.
- ↑ Chase, M.W. and H.G. Hills. 1991. Silica gel: An ideal material for field preservation of leaf samples for DNA studies. Taxon 40:215–220.
- ↑ Nagy, Z.T. 2010. A hands-on overview of tissue preservation methods for molecular genetic analyses. Organisms Diversity & Evolution 10:91–105.
- ↑ Corthals, A. 2006. The Ambrose Monell Cryo-Collection: A museum-based molecular collection. Pp. 107–113 in DNA and Tissue Banking for Biodiversity and Conservation: Theory, Practice and Uses (V. Savolainen, M.P. Powell, K. Davis, G. Reeves, and A. Corthals, eds.). Kew Publishing, Royal Botanic Garden, Kew,England. 151 pp.
- ↑ Corthals, A. and R. DeSalle. 2005. An application of tissue and DNA banking for genomics and conservation: The Ambrose Monell Cryo-Collection (AMCC). Systematic Biology 54:819–823.
- ↑ Johnson, B. 1999. Frozen in time: Ultra low freezers, dewars, and tubes. The Scientist 13(1):19.
- ↑ Cable, S. and T.K. Fulcher. 2006. Databasing and information technology. Pp. 61–65 in DNA and Tissue Banking for Biodiversity and Conservation: Theory, Practice and Uses (V. Savolainen, M.P. Powell, K. Davis, G. Reeves, and A. Corthals, eds.). Kew Publishing, Royal Botanic Garden, Kew, England. 151 pp.
- ↑ Coddington, J., K. Barker, G. Droege, J.J. Astrin, P. Bartels, C. Butler, D. Cantrill, F. Forest, B. Gemeinholzer, D. Hobern, J. Mackenzie-Dodds, E.O. Tuama, G. Petersen, O. Sanjur, D. Schindel, and O. Seberg. 2014. GGBN: Making genomic collections discoverable for research through a networked community of biodiversity repositories. Pp. 165–168 in DNA Banking for the 21st Century. Proceedings of the U.S. Workshop on DNA Banking (W.L. Applequist and L. Campbell, eds.). William L. Brown Center, St. Louis, Missouri. 187 pp.
- ↑ Renner, S.C., D. Neumann, M. Burkart, U. Feit, P. Giere, A. Gröger, A. Paulsch, C. Paulsch, M. Sterz and K. Vohland. 2012. Import and export of biological samples from tropical countries — Considerations and guidelines for research teams. Organisms Diversity & Evolution 12:81–98.
- ↑ Moore, G.K. and W. Tymowski. 2005. Explanatory guide to the International Treaty on Plant Genetic Resources for Food and Agriculture. IUCN Environmental Policy and Law Paper No. 57. IUCN, Gland, Switzerland. 212 pp.
- ↑ Davis, K., C. Williams, M. Wolfson, and J. Donaldson. 2006. Practical implementation of the CBD and CITES. Pp. 36–46 in DNA and Tissue Banking for Biodiversity and Conservation: Theory, Practice and Uses (V. Savolainen, M.P. Powell, K. Davis, G. Reeves,and A. Corthals, eds.). Kew Publishing, Royal Botanic Garden, Kew, England. 151 pp.
- ↑ Donaldson, J. 2006. CITES and DNA banking. Pp. 30–35 in DNA and Tissue Banking for Biodiversity and Conservation: Theory, Practice and Uses (V. Savolainen, M.P. Powell, K. Davis, G. Reeves, and A. Corthals, eds.). Kew Publishing, Royal Botanic Garden, Kew, England. 151 pp.
- ↑ 33.0 33.1 33.2 Applequist, W. 2014. Legal and ethical issues related to DNA banking. Pp. 137–146 in DNA Banking for the 21st Century. Proceedings of the U.S. Workshop on DNA Banking (W.L. Applequist and L. Campbell, eds.). William L. Brown Center, St. Louis, Missouri. 187 pp.
- ↑ Kapinos, E. and S. Graham. 2006. DNA banking and health, safety and security. Pp. 52–60 in DNA and Tissue Banking for Biodiversity and Conservation: Theory, Practice and Uses (V. Savolainen, M.P. Powell, K. Davis, G. Reeves, and A. Corthals, eds.). Kew Publishing, Royal Botanic Garden, Kew, England. 151 pp.
- ↑ Secretariat of the Convention on Biological Diversity. 2011. Nagoya Protocol on Access to Genetic Resources and the Fair and Equitable Sharing of Benefits Arising from Their Utilization to the Convention on Biological Diversity. Secretariat of the Convention on Biological Diversity, Montreal, Canada. 25 pp. http://www.cbd.int/abs/doc/protocol/nagoya-protocol-en.pdf (1 November 2014).